19th World Congress on Menopause
19th World Congress on Menopause will be held in Melbourne on 19-22 October 2024.
Due to the overwhelming success of IMS2024, registrations have now reached full capacity and are officially closed.
We look forward to welcoming all registered attendees to an exciting event!
Missed Out? Join IMS2024 On Demand!
For those who couldn’t secure an on-site spot, we’ve got great news: IMS2024 On Demand. This gives you the chance to experience all sessions from the congress at your own pace.
How It Works:
- Purchase Credits: Buy the credits needed to access the On Demand content.
- Select Your Sessions: Choose from the available sessions based on your interests.
- Watch the Videos: Credits will be deducted as you access each session.
Lectures will be available for 12 months from November 11th, 2024, allowing you ample time to explore all the content.
Not Sure How Many Credits to Purchase?
Check the program to estimate how many credits you might need. Don’t worry - you can always add more credits at any time!
Learn more and see the FAQs at https://imsmelbourne2024.com/ondemand/
Pre-congress course: Menopause Essentials Update - Friday October 18th 2024 13:30–18:00
AMS announces its popular MENOPAUSE ESSENTIALS UPDATE on October 18th at 1.30-6pm.
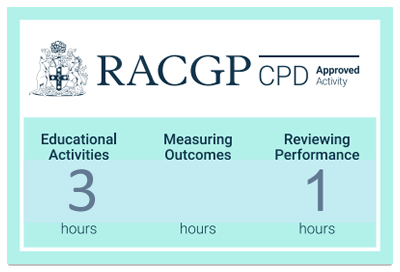
You are eligible for CPD points by attending of 3 hours EA and 1 hour RP.
It gives you menopause management at your fingertips. $150 - join here.
Where and When
The pre-congress courses will be held at the Room 203 at the Melbourne Convention and Exhibition Centre on 18 October 2024 from 13:30 to 17:30.
Note: This course will not be available online. In person attendance is required.
Registration
The pre-congress course is not included with the congress registration fee. In order to participate you are required to purchase it separately. The course costs $150.
Limited spots are available.
Course Overview
Menopausal symptoms can impact women's lives dramatically. Participating in the 19th IMS World Pre-Congress Menopause Essentials Update offers healthcare providers an invaluable opportunity to stay updated with the latest advancements and best practices in menopause care. This event equips participants with practical knowledge and strategies that can be directly applied in clinical settings. This can support them to deliver comprehensive care and empower patients to manage their symptoms during this transition.
Learning Outcomes
- Describe how to diagnose and manage menopause within a structured consultation in primary healthcare setting.
- Identify the benefits and risks of menopausal hormone therapy.
- Describe the different non-hormonal treatment options for the symptoms of menopause.
- Describe how to tailor treatment for complex cases to ensure patient safety.
CPD Points
RACGP CPD
ACRRM CPD
The Pre-Congress Menopause Essentials Update is an accredited ACRRM CPD activity 34502. It has been approved for:
- 3 hours Educational Activity (EA)
- 1 hour Outcome Measurement (OM)
If you require an ACCRM certificate of attendance, you must include your seven-digit ACRRM number and surname in your IMS profile. Badge scanning at least once per day is also required for all CPD accreditation.

RANZCOG CPD
The Pre-Congress Menopause Essentials Update has been approved has been approved for the following RANZCOG CPD, Domains & hours: Educational Activity Hours: 3.00, Outcome Measurement Hours: 1.00
Please note, if the activity meets more than one domain these will need to be logged separately in the CPD portal.
Meets program level requirement/s: Professionalism.

Speakers
 |
Dr Jane ElliottMenopause consultation: a structured approach
|
An introduction to the basic physiology of menopause, definitions of menopause and how to diagnose menopause. I will discuss why it is usually unhelpful to use hormone blood tests to diagnose menopause in the normal age range of 45 to 55 years. It will provide a practical structure of how to conduct an initial menopause consultation and the factors to be taken into account in the history. As well as symptoms of menopause I will discuss the ongoing health consequences of menopause that need to be considered in a menopause consultation. The talk will be clinically practical for all family medicine specialists and non-family medicine specialists.
 |
Prof Susan Davis AOPrescribing MHT: practical and evidence-based approach to treatment |
Menopausal hormone therapy (MHT) describes the systemic administration of sex steroids to women with ovarian insufficiency following natural or surgical menopause, and premature ovarian insufficiency (POI). Similar regimens are also used for women with hypothalamic amenorrhoea and ovarian insufficiency secondary to hypopituitism. MHT is not transgender therapy, although the formulations used may be the same. MHT refers to oestrogen with or without a progestogen, but now also includes oestrogen with bazedoxifene (a selective oestrogen receptor modulator [SERM]) and tibolone (a steroid that exerts oestrogenic, progestogenic and androgenic effects). As testosterone therapy is not a first line therapy postmenopausal therapy it is not generally included in MHT but rather as androgen therapy. The term “progestogen” includes all therapies with progestational uterine effects and is an umbrella term for progesterone and the synthetic progestogens which are referred to as progestins. The primary indications for oestrogen therapy are symptoms relief and prevention of bone loss and fragility fracture. Oestrogen should be co-prescribed with a progestogen unless the patient has had a hysterectomy. Inclusion of a progestogen should be considered if women have had recent severe endometriosis or a subtotal hysterectomy. MHT is available in multiple formulations and doses, allowing for treatment individualisation. Patients should be advised that dose adjustment and/or trialling of different formulations is often needed to optimise the benefits without side effects. While there is substantial emphasis on “body identical” hormone therapy and nonoral oestrogen, synthetic progestogens and oral oestrogens still have an important role and provide many women with the best therapeutic effects. Understanding what options might be best used in different settings and the pros and cons of different formulations will achieve the best patient outcomes.
Afternoon Tea
 |
Dr Premitha DamodaranNon-hormonal options for managing troublesome symptoms of menopause |
Women deserve the freedom to choose how they manage their perimenopausal and menopausal symptoms. For those who cannot or prefer not to use menopausal hormonal therapy (MHT), nonhormonal options are available. This includes women with contraindications to MHT, such as those with estrogen-related cancers, a history of venous thromboembolism, strokes, coronary heart disease, thrombophilia, or those who are intolerant or simply opt out of MHT. Lifestyle modifications are foundational in managing menopause. Obesity, for instance, can exacerbate vasomotor symptoms, while a healthy diet and regular exercise help reduce inflammatory visceral fat, benefiting heart health, bone strength, and overall mobility. Reducing alcohol, smoking, vaping, spicy foods, and caffeine can also improve overall well-being. Equally important, good sleep hygiene is crucial for reducing fatigue, brain fog, and aiding in weight management. A new addition to nonhormonal therapy is Fezolinetant, an NK3 receptor antagonist that effectively treats vasomotor symptoms by modulating neuronal activity in the brain's thermoregulatory zone. Herbal products such as black cohosh, soy-based and plant estrogens, and evening primrose oil have not shown significant benefits for vasomotor symptoms, sleep, or other menopausal challenges. Instead, evidence-based treatments like cognitive behavioural therapy (CBT) and hypnotherapy, supported by Level 1 evidence, have shown meaningful improvements in vasomotor symptoms, sleep disturbances, and anxiety. Other nonhormonal treatments include clonidine, gabapentin, pregabalin, SSRIs, and oxybutynin, though each comes with its own side effects. For managing genitourinary syndrome of menopause, nonhormonal options include vaginal lubricants, moisturizers, and local anaesthetic creams. Additionally, low-dose vaginal estrogen creams and tablets can be used to maintain vaginal health.
 |
Dr Sonia DavisonCase studies: a discussion of complex cases and referral pathways in primary care |
MHT in the setting of co-morbidities In general, hormone therapy (MHT) is first line pharmacological management for women with significant menopausal symptoms. While there are relatively few contraindications to MHT when compared with synthetic hormones, in the setting of certain co -morbidities, the majority of professional organisations and guidelines discourage the use of MHT in favour of non hormonal management. This presentation is case based and will discuss evidence for use or avoidance of MHT when a woman presenting with significant symptoms attributable to menopause has a pre existing history of VTE, endometriosis, menstrual migraine with or without aura, breast cancer, or a BRCA mutation.
Content updated October 2024


