Perimenopause or Menopausal Transition
Key Points:
|
![]() AMS The Perimenopause or Menopausal Transition265.51 KB
AMS The Perimenopause or Menopausal Transition265.51 KB
What is perimenopause?
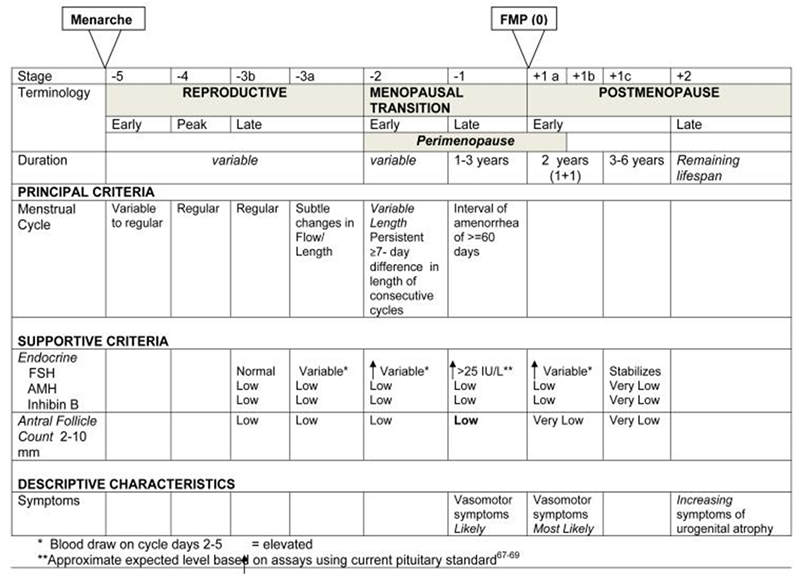
The perimenopause is the reproductive phase in a woman’s life occurring before the final menstrual period, or menopause. The Stages of Reproductive Aging Workshop (STRAW +10) system is a defined set of nomenclature which describes the stages of ovarian ageing (Figure 1). Based on these criteria, perimenopause starts when there are persistent differences in cycle length of seven or more days between consecutive cycles (Stage -2) and continues until 12 months after the last menstrual period (stage +1a) (1).
These criteria can be difficult to apply to women who use hormonal contraception, have had an endometrial ablation or hysterectomy. In these women perimenopause is heralded by typical menopausal symptoms. For women less than 45 years of age, FSH testing is recommended, but for women older than 45 diagnostic blood tests including FSH are not necessary (2).
Figure 1: The Stages of Reproductive Aging Workshop (STRAW +10) criteria
Symptoms and Assessment
Perimenopausal symptoms include both those associated with oestrogen excess, and oestrogen deficiency. Symptoms of oestrogen excess can include mastalgia, heavy menstrual bleeding and headaches. The symptoms of oestrogen deficiency include vasomotor symptoms, sleep disturbance, mood changes, fatigue, cognitive concerns, low libido, genitourinary symptoms, arthralgia and myalgia (2).
Perimenopause is also a time when risk factors for chronic disease change. This includes acceleration of bone loss, increase in cardiovascular risk factors including central adiposity, adverse changes in lipids and altered glucose metabolism (2). There is an increased incidence of mood disorders, especially for those women who have a history of hormone related mood symptoms (3). Cancer screening programs including bowel, breast, and cervical cancer should also be discussed.
A structured approach to the perimenopause consult is recommended. This allows the practitioner to establish the diagnosis, review symptoms and concerns, and address chronic disease risk factors. An individualised treatment plan can then be established for each patient. This should be regarded as an opportunity to offer lifestyle recommendations, health promotion and screening advice in a woman’s midlife.
Management of Symptoms
Menopausal Symptoms
MHT is the most effective treatment option for menopausal symptoms (4). With the exception of women with contraindications, MHT should be offered to those reporting bothersome symptoms (see AMS Information Sheets Combined MHT, Oestrogen only MHT and Risks and benefits of MHT) . Lifestyle advice remains important for all women (see AMS Information Sheet Lifestyle and behaviour modifications for menopausal symptoms). For those women unable to use MHT there are non-hormonal treatments which should be discussed (See AMS Information Sheet Non-hormonal treatments for menopausal symptoms). For those with an intact uterus, MHT is prescribed in a cyclical or sequential regime in the perimenopause, using the lowest effective dose of oestrogen. Oral and transdermal continuous regimes are not recommended due to the high incidence of unscheduled bleeding (See AMS Information Sheet AMS guide to MHT/HRT equivalent doses Australia only and AMS guide to MHT/HRT equivalent doses New Zealand only). The 52mg levonorgesterol intrauterine device (IUD) is an excellent option for both endometrial protection and contraception during the perimenopause. Women who have had a hysterectomy do not require a progestogen.
Bleeding
Many women experience menstrual irregularities during the perimenopause due to fluctuating oestrogen levels. Bleeding should be investigated when it is very heavy, post-coital, prolonged, or if it occurs after 12 months of amenorrhoea. (See AMS Information Sheet Bleeding – perimenopausal, postmenopausal and breakthrough bleeding on MHT/HRT). Abnormal pathology must be excluded before MHT is prescribed. The 52mg levonorgestrel IUD is highly effective in managing heavy or irregular bleeding. The progesterone only pill can also be used; the drospirenone only formulation is associated with lower rates of unscheduled bleeding or spotting (5). Other options include the combined oral contraceptive pill (COCP) if appropriate. Tranexamic acid, as a fibrinolytic agent and not a hormonal agent, is taken just with the heavy bleeding and reduces it by up to 50 %. In more severe cases, endometrial ablation or even hysterectomy may be considered.
Mood Concerns
Perimenopause is a window of vulnerability for the development of depressive symptoms and major depressive episodes. This can occur in women with no history of a mood disorder, but those at highest risk are women with a history of a major depressive disorder, and hormone related mood disorders. Mood symptoms need full assessment and a multimodal approach, including psychological therapy and lifestyle advice. Antidepressant pharmacotherapy and MHT can be considered as treatment options for some women (see AMS Information Sheet Mood and the menopause) (3).
Contraception
Women may still be having ovulatory cycles during the perimenopause and need to be counselled about the need for contraception. For women under 50 years of age, contraception is required for 2 years after their last menstrual period. For women over 50 years of age this is reduced to 1 year (6). Amenorrhea is common in perimenopausal women using progesterone-only contraception making it difficult to determine the date of her FMP. In this situation, for women age 50 or older, a single FSH measurement ≥30IU/L will indicate that contraception will be required for a further 12 months, and can then be ceased. If the FSH is ≤30IU/L, contraception should be continued for the next 12 months and FSH to be repeated to check if ≥30 at that time (See AMS Information Sheet Contraception) (7).
References
- Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, Sherman S, Sluss PM, de Villiers TJ. STRAW+10 Collaborative Group. Executive summary of the Stages of Reproductive Aging Workshop +10: addressing the unfinished agenda of staging reproductive aging. Climacteric. 2012 Apr;15(2):105-14.
- Magraith K, Stuckey B, Baber R. Perimenopausal Hormone Therapy Assessment and Prescribing. Medicine Today. 2022 August (23):61-67
- Maki PM, Kornstein SG, Joffe H, Bromberger JT, Freeman EW, Athappilly G, Bobo WV, Rubin LH, Koleva HK, Cohen LS, Soares CN. Guidelines for the Evaluation and Treatment of Perimenopausal Depression: Summary and Recommendations. J Womens Health (Larchmt). 2019 Feb;28(2):117-134.
- Hamoda H, Panay N, Pedder H, & Arya R, Savvas M. The British Menopause Society and Women’s Health Concern 2020 Recommendations on Hormone Replacement Therapy in Menopausal Women. consensus statement 2020. Post Reprod Health. 2020 Dec;26(4):181-209
- Chiara Del Savio M, De Fata R, Facchinetti F, Grandi G. Drospirenone 4 mg-only pill (DOP) in 24+4 regimen: a new option for oral contraception. Expert Rev Clin Pharmacol. 2020 Jul;13(7):685-694.
- Sauer MV. Reproduction at a advanced maternal age. Fertility Sterility. 2015; 103(5):1136-43
- Faculty or Sexual and Reproductive Healthcare. FSRH Guideline for women aged over 40 years. Contraception for Women aged over 40 years. FSRH Clinical Effectiveness Unit; 2017(Amended 2019. (To download: https://www.fsrh.org/standards-and-guidance/documents/fsrh-guidance-contraception-for-women-aged-over-40-years-2017/ )

Note: Medical and scientific information provided and endorsed by the Australasian Menopause Society might not be relevant to a particular person's circumstances and should always be discussed with that person's own healthcare provider. This Information Sheet may contain copyright or otherwise protected material. Reproduction of this Information Sheet by Australasian Menopause Society Members and other health professionals for clinical practice is permissible. Any other use of this information (hardcopy and electronic versions) must be agreed to and approved by the Australasian Menopause Society.
Content updated March 2023
