Diagnosing Menopause
Key Points
|
![]() Diagnosing_menopause.pdf147.55 KB
Diagnosing_menopause.pdf147.55 KB
DON’T
- Measure FSH, LH, AMH (anti-Müllerian hormone), oestradiol or testosterone, inhibin A or B (which inhibit FSH production) levels and antral count or ovarian volume in a woman with symptoms at the normal age for menopause (over 45 years) because these results are unlikely to change your management. The indications for intervention are clinical.
BUT for premature menopause
- Which is defined as occurring before the age of 40 and is designated as ‘Premature Ovarian Insufficiency’ (POI).
- Measurement of FSH is indicated in women under 40 and 40-45 with menopausal symptoms. Premature menopause is diagnosed by elevated FSH levels on two occasions, 4-6 weeks apart.
DO take a history
- Menopausal symptoms – the multiplicity of which are identified in the Greene scale below is a useful standardised symptom measurement system.
- Vasomotor symptoms cause sleep disturbance. Ask about severity and number.
- Sleep disturbance is a major factor affecting quality of life. Identify the impact of sleep disturbance.
- Record personal medical history and risk factors for breast cancer, cardiovascular disease, thromboembolic disease and osteoporosis.
- Ask about absolute or relative contraindications to MHT: uncontrolled hypertension, undiagnosed abnormal bleeding, previous breast or endometrial cancer and personal history or high inherited risk of thrombo-embolic disease
- Ensure that screening (breast, cervical) is up to date
Introduction
Frequently, the woman herself has already made the diagnosis of menopause. She attends her doctor with symptoms such as hot flushes or night sweats interrupting her sleep, together with changes in her menstrual cycle. Not all women with menopausal symptoms will need treatment. Most women will be glad of information about menopause and about the safe and effective treatment options available. The questions we should be asking her are "Why did you come to see me", and "What do you hope to get out of this consultation?"
Common questions are:
- How long does menopause last?
- When will I be through it?
- What are the pros and cons of taking menopause hormone therapy (MHT) for me?
- Can I treat my symptoms naturally?
- If I do decide to take MHT, for how long should I take it?
- When am I no longer fertile and when should I stop using contraception?
There is a lot of information to give, and even if a menopause information sheet is given, a long appointment will be required to give all the information required and answer questions. Menopausal women often have multiple health issues that need addressing and they may be anxious and tired due to sleep disturbance. Allowing adequate time for the consultation allows her to discuss the issues she is concerned about without feeling rushed.
Perimenopause, Menopause or Postmenopause?
Perimenopause refers to the time from the onset of menopausal symptoms (some or all of symptoms such as irregular periods, hot flushes, night sweats or sleep disturbance) to 12 months after the last menstrual period1. This can last on average 4 to 8 years. Menopause is the last menstrual period. One year after the last menstrual period the woman is considered "postmenopausal". Peri-menopausal symptoms can occur when periods are still regular, but typically the symptoms worsen in the premenstrual days. The symptoms experienced during the perimenopause are often the most distressing. Menstrual changes are common and it is normal to have periods that are less frequent or irregular. More frequent periods or those that are very heavy may not be normal and suggest that there may be pelvic or systemic pathology.
Women older than 40 years with more frequent or heavy bleeding, or intermenstrual bleeding require investigation by their doctor. Hormone levels may fluctuate during this time and measurement of sex steroids is rarely clinically helpful once the diagnosis has been made2. At this time of hormone fluctuation, oestradiol can actually briefly be higher than normal, giving symptoms of excess oestrogen, such as breast tenderness. Explaining to women that, at a time when their body is running out of oestrogen, they may get brief periods of high oestrogen symptoms is useful. (Some women are told that because of these brief periods of high oestrogen they need progesterone treatment but there is no evidence that this is needed). Eventually, symptoms of oestrogen deficiency predominate.
Menopause is said to have occurred when there has been no menstruation for one year. If a woman has taken MHT since she was peri-menopausal, it may not be possible to assess the exact age at which she became menopausal. This may also impact on the advice provided about perimenopausal contraception (see AMS information sheet Contraception) If a woman has required peri-menopausal MHT for symptoms, it is a reasonable guess to expect her to be post-menopausal after 4-5 years.
Postmenopause
This starts one year after the last menstrual period. There is no reliable way of predicting how long menopausal symptoms will continue. For many women they resolve within 2-5 years. Ten to 20% of women will have symptoms for up to 12 years. Vaginal dryness and urinary frequency may start during the peri-menopause and tend not to resolve naturally with time. Some women only experience vaginal dryness during sexual activity and others are aware of uncomfortable vaginal symptoms at other times.
For those symptomatic women who elect to use MHT, we advise that they be reviewed annually to evaluate ongoing care and the need to continue MHT.
Premature menopause
Premature menopause is considered to have occurred if a woman is younger than 40 when she becomes menopausal. About 1% of women experience a spontaneous premature menopause (POI or premature ovarian insufficiency) and around another 6% have premature menopause due to surgery, chemotherapy or radiation. There has been relatively little research on symptoms in these women, but it seems that their menopausal symptoms may be more severe than in older women, particularly when menopause occurs due to surgery or chemotherapy. There are also distinct personal, sexual, social and psychological issues for younger women, particularly for those women who wish to have children but have not yet started or completed their families. These women need extra counselling, and time to come to terms with their situation. This is the one time that measuring and finding a high FSH and a low oestradiol is helpful to differentiate between menopause and other causes of secondary amenorrhoea.
- POI is a pathological condition associated with an increased risk of osteoporosis and fracture, an increased risk of cardiovascular disease, possible cognitive impairment, Parkinson’s disease and reduced life expectancy. It is conventional to treat with MHT at least until the average age of the menopause.
- There are 3 main identifiable causes of POI: genetic, autoimmune and iatrogenic3
- Genetic conditions include a strong maternal family history, 45,X, 46,XX and46,XY POI.
- POI is associated with galactosemia and FMR premutations (e.g., Fragile X)
- Women with an autoimmune predisposition may develop autoimmune POI, with or without other autoimmune diseases (diabetes mellitus, Addison's, thyroid).
- Women with iatrogenic menopause includes women with benign disease and those having treatment for cancer (hormonal, chemotherapy and/or radiotherapy) which has brought about an early menopause. In most women the cause of an early menopause is unknown.
- Early menopause affects 3.7% of African-American women, 2.9% of white women, 2.2% of Chinese women and 0.8% of Japanese women4. About 1 in 1000 women are affected under the age of 305.
- Lower socioeconomic status has been associated with POI.
The measurement of FSH and oestradiol should be repeated at least once (See AMS information sheets Early Menopause Due to Chemotherapy and Spontaneous Premature Ovarian Insufficiency).
Symptom assessment and diagnosis at Perimenopause and Menopause
The time when most women are trying to understand what is happening to them is during the peri- menopause. During this time of hormonal fluctuation women may experience some, but not all of the symptoms listed in the table. For instance, she may come with severe joint aches and tiredness, which may be suggestive of a rheumatological disease. Checking a symptom score will often reveal many more unreported menopausal symptoms.
In most cases, recording a symptom score helps to make the diagnosis, at the same time educates the woman and is a basis for assessing efficacy of treatment. Checking FSH or AMH levels or serum oestradiol and progesterone are unnecessary tests in diagnosing menopause for most women. Checking an androgen profile as a routine on all peri-menopausal women is also unnecessary and costly. Many women come to the consultation expecting a blood test to diagnose menopause, and it is important to explain to them why we use the symptom score rather than a blood test in establishing a diagnosis. It is important to explain to women that the blood tests of FSH/oestradiol can fluctuate on a daily basis and therefore are not useful or necessary. It is especially unhelpful to do hormone blood tests while women are on MHT/OCP – symptoms, not blood levels, guide therapy. Treat the symptoms, not the biochemistry.
Symptom score sheet
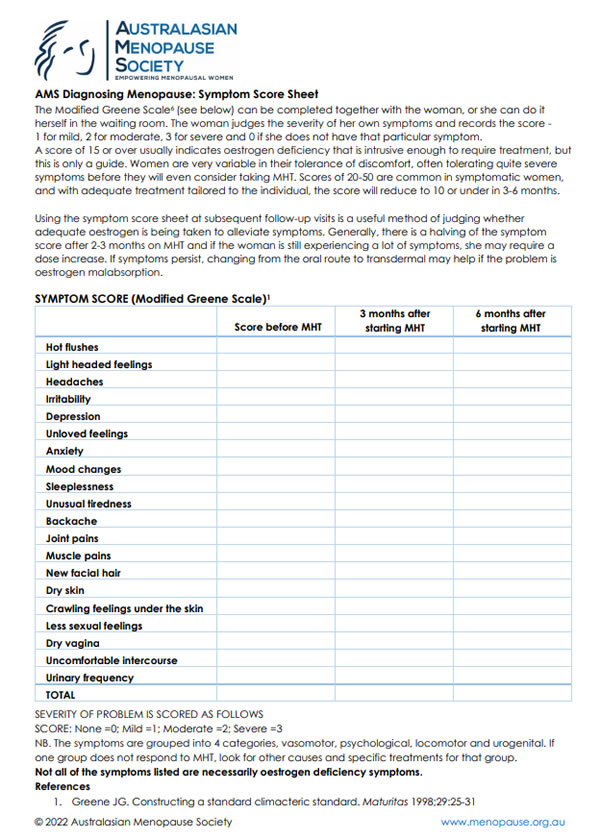
The Modified Greene Scale6 (see below) can be completed together with the woman, or she can do it herself in the waiting room. The woman judges the severity of her own symptoms and records the score - 1 for mild, 2 for moderate, 3 for severe and 0 if she does not have that particular symptom. A score of 15 or over usually indicates oestrogen deficiency that is intrusive enough to require treatment, but this is only a guide. Women are very variable in their tolerance of discomfort, often tolerating quite severe symptoms before they will even consider taking MHT. Scores of 20-50 are common in symptomatic women, and with adequate treatment tailored to the individual, the score will reduce to 10 or under in 3-6 months.
Using the symptom score sheet at subsequent follow-up visits is a useful method of judging whether adequate oestrogen is being taken to alleviate symptoms. Generally, there is a halving of the symptom score after 2-3 months on MHT and if the woman is still experiencing a lot of symptoms, she may require a dose increase. If symptoms still persist, changing from the oral route to transdermal may help if the problem is oestrogen malabsorption.
If it's not menopause, what is it?
Depression, anaemia and thyroid disorders are the most common conditions that may occur concurrently. Unstable diabetes and hyperthyroidism may cause hot flushes. Medication, such as the SSRI family of anti-depressants, may also cause hot flushes.
Doing a blood count, ferritin and/or a TSH level will usually establish the diagnosis. However, if a woman presents with low mood or anxiety, there is a need to evaluate whether this is a primary anxiety/depression or one aggravated by the lack of oestrogen. A previous history of depression or an elevated FSH may help to differentiate between the two. Hair loss may be a sign of iron deficiency or hypothyroidism rather than menopause.
Need more information?
Diagnosing menopause is something that most GPs are skilled at doing and helping women at this difficult stage of their life can be very rewarding. If you are reading this information sheet because you have inadequate knowledge on how to counsel menopausal women, then consider joining the Australasian Menopause Society and receiving its monthly newsletter, called eChanges. Attend one of our annual meetings, which aim to be of interest to a wide range of doctors, nurses, psychologists and physiotherapists.
References
- McKinlay SM et al. The normal menopause transition. Maturitas 1992;14:103.
- Burger HG. Unpredictable endocrinology of the menopause transition: clinical, diagnostic and management implications. Menopause Int 2011;17:153.
- Şükür, Y[anuz]. E., Kıvançlı, İ. B., & Özmen, B. Ovarian aging and premature ovarian failure. Journal of the Turkish German Gynecological Association, 2014;15(3):190.
- Green R et al. Menopausal Symptoms and Ethnicity: the Study of Women’s Health across the Nation. Womens Health (Lond). 2009;5(2):127-33
- Coulam CB et al. Incidence of Premature Ovarian Failure. Obstet Gynecol 1986;67(4):604-606
- Greene JG. Constructing a standard climacteric standard. Maturitas 1998;29:25-31
Symptom Score (Modified Greene Scale)
![]() AMS Diagnosing Menopause Symptom score sheet91.45 KB
AMS Diagnosing Menopause Symptom score sheet91.45 KB

Note: Medical and scientific information provided and endorsed by the Australasian Menopause Society might not be relevant to a particular person's circumstances and should always be discussed with that person's own healthcare provider. This Information Sheet contains copyright or otherwise protected material. Reproduction of this Information Sheet by Australasian Menopause Society Members and other health professionals for clinical practice is permissible.
No other reproduction or transmission is permitted in any form or by any information storage and retrieval systems except as permitted under the Copyright Act 1968 or with prior written permission from the copyright owner.
Content created May 2022
